Share:
One of the ultimate goals for benefits leaders is to deliver better experiences—from the way people access their benefits, to how they engage with each vendor, to the value they ultimately get out of it.
But a common obstacle is that these experiences are often fragmented. This leaves employees feeling siloed and minimizes their connection with the benefits their employers are offering to them.
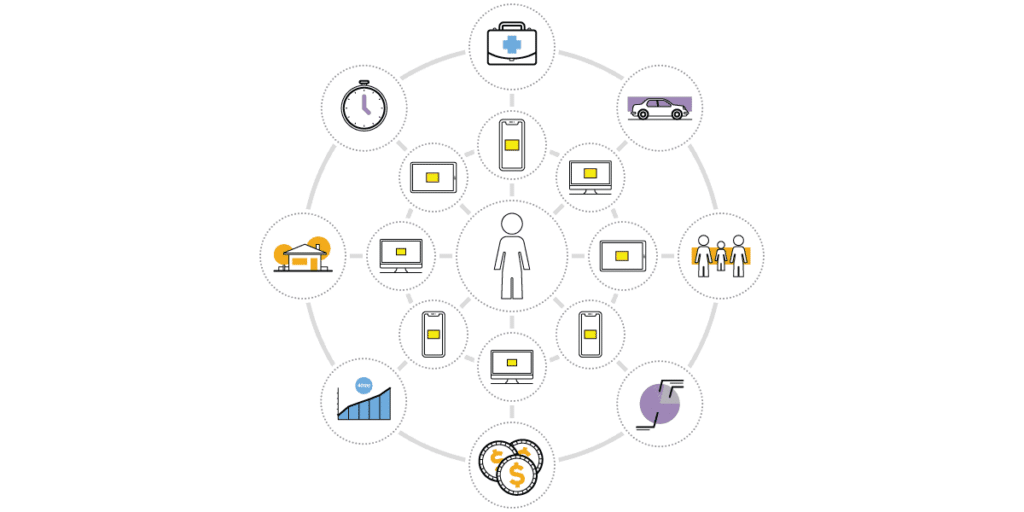
The best way to unify these experiences—and deliver value throughout the employee journey—is through a single, powerful, data-driven platform. When you have that single source of intelligence that drives recommendations for an ever-evolving personal profile, the benefits experience becomes interconnected across all your channels and vendors.
Just like that, benefits become a seamless part of everyday life. Here’s how:
One point of entry
My previous post about the siloed benefits experience examined a few different scenarios employees could encounter. From visiting an onsite clinic to seeking telephonic support to engaging with a vendor portal, we saw the complicated journey, full of barriers, that people typically have to go through.
However, by using a digital engagement platform like MyEvive that makes all of their benefits accessible, people can accomplish all of their tasks. Just by logging in once, they’re equipped to interact with each vendor and have a bevy of tools at hand. They can pull up their health insurance card at their doctor’s office; they can get clarification on their coverage; they can easily connect to their 401(k) accounts, view their HSA balance, and more.
Employees also need to be able to reach this main access point from anywhere. That’s why MyEvive meets people where they are: on their laptops at home, on a mobile app while they’re out and about, or via SMS reminders and notifications they’ve opted into.
The right guidance for a unified experience
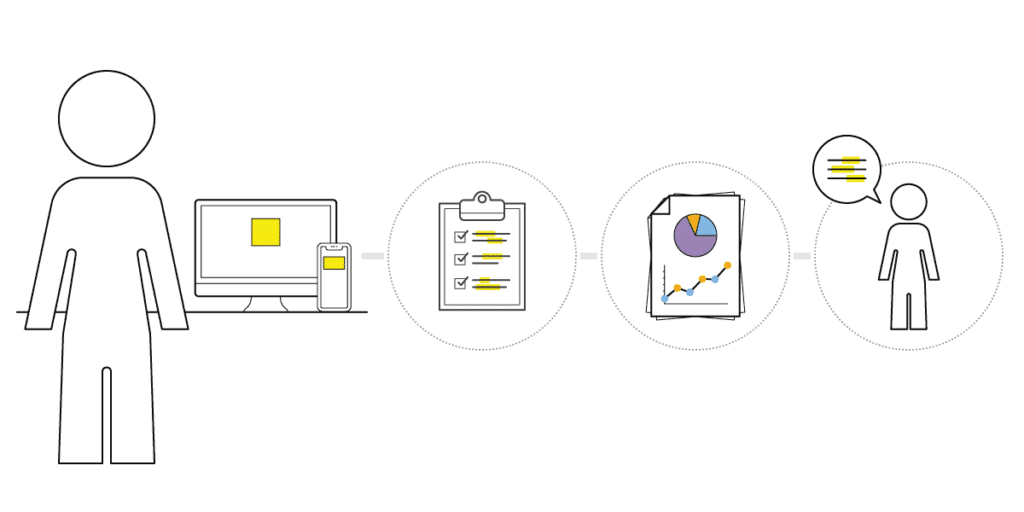
When you connect and integrate your data streams through a system of intelligence like the Evive Operating System (eOS), you can give your employees personalized recommendations that’ll improve their overall experience—and their outcomes.
The true power of such a data-driven system is that it leverages data from the many systems of record and systems of engagement in your benefits ecosystem. Apply predictive analytics, and you can generate relevant and timely messaging directing the right person to the right resource at the right time.
Here’s what this looks like in action:
An employee receives notifications generated by eOS, through his MyEvive app, about onsite clinics where he can get biometric screenings. He ends up doing this and learns he has diabetes. MyEvive not only displays the results from his lab, but nudges him toward the next step—finding a high-quality, in-network endocrinologist—and connects him to a provider-search tool that he can use. From there, the data-driven guidance of eOS uses his ensuing health claims to remind him of his ongoing chronic care on the right schedule, and also keeps him engaged with both his health plan’s advocacy program and his available diabetes management program.
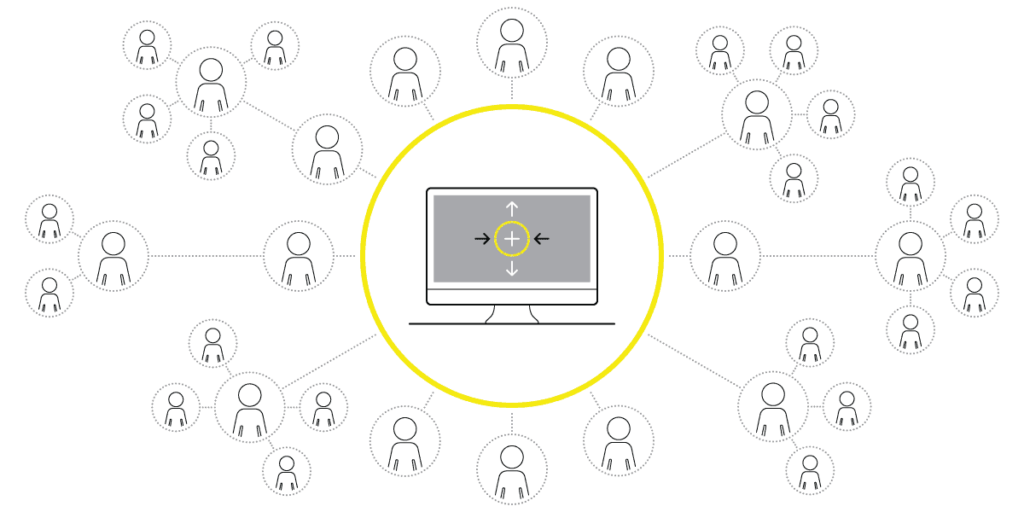
Empowering vendors to coordinate care
What about later down the line, when our example employee calls his pharmacy benefits manager (PBM) with questions about diabetes medication? In the typically fragmented, siloed experience, the PBM representative who takes his call wouldn’t know the employee’s company offers a weight-loss program that could help him control his diabetes, and thus, a teachable moment would be missed.
An experience like this needs to be interconnected as well. That’s where Evive 360 comes in. This application allows advocates, benefits concierges, onsite care providers, and other vendors to see relevant insights about the member journey, including past interactions and screenings, messaging they’ve received, and missed or upcoming opportunities.
With Evive 360 integrated into the PBM’s customer-relationship management software, the representative in this scenario sees the eOS-generated recommendation for the weight-loss program that’s available to the employee. While answering the question about medication, the rep can refer to the program as another available resource.
A unifying solution
Solutions like MyEvive and Evive 360, powered by a system of intelligence like eOS, ultimately reduce barriers to engagement, bring more value to every touchpoint, and give employees one streamlined benefits experience.
The benefits you’ve thoughtfully put together are still there—only now they can work together, bringing more value to you and your employees.






