Evive makes it easy.
Looking to increase benefits utilization + engagement? Leave the heavy lifting to us. As experts in data and HR, we've built powerfully personalized, ready-to-go campaigns that reach employees with the information they need, when it matters most.




Does personalization drive better employee engagement? Our latest survey says yes!
Every employee is unique. Their benefits experience should be, too.
Using data from diverse sources, Evive creates robust employee profiles that enable us to send expertly-crafted, personalized messages about the right benefits at just the right time. Built and refined by our experts over 17 years, the platform continually ingests and learns new information in a data-driven, closed-loop system, ensuring employees automatically receive only relevant communications about the benefits that matter most to them. What’s more, our business-ready solution requires little effort from your team, freeing up vital HR resources to focus on other priorities.


Supercharge your people strategy
Who We Serve
Employers
Managing a massive workforce can spell major engagement challenges for large employers. Evive’s highly configurable solution has helped some of the biggest brands boost benefits utilization, improve engagement, and achieve better business outcomes.
Channel
Benefits are meaningless if employees don’t use them. Evive’s proven messaging technology amplifies enrollment and engagement in a wide range of programs, from point solutions to healthcare accounts.
Consultants + Brokers
Benefits consultants help employers make sense of an increasingly complex benefits landscape, developing strategies and guiding clients towards needed solutions. Evive helps you make those strategies a reality, and deliver measurable results to your clients.
The Power Of Data + Personalization
Over our 15 years in business, we’ve built an agile, industry-leading engagement solution that’s changed how companies communicate—and improved the financial, physical, and emotional well-being of their workers.
A Culture Of Passion + Innovation
Evivers are creative, collaborative, and committed to optimizing the employee experience. If this sounds like you, and you’re interested in bringing your talents to a fast-paced company that values your voice and gives you room to grow, let’s talk.
Our Customers Inspire Us












Ready to see how we replace sweat with software? Request a demo.
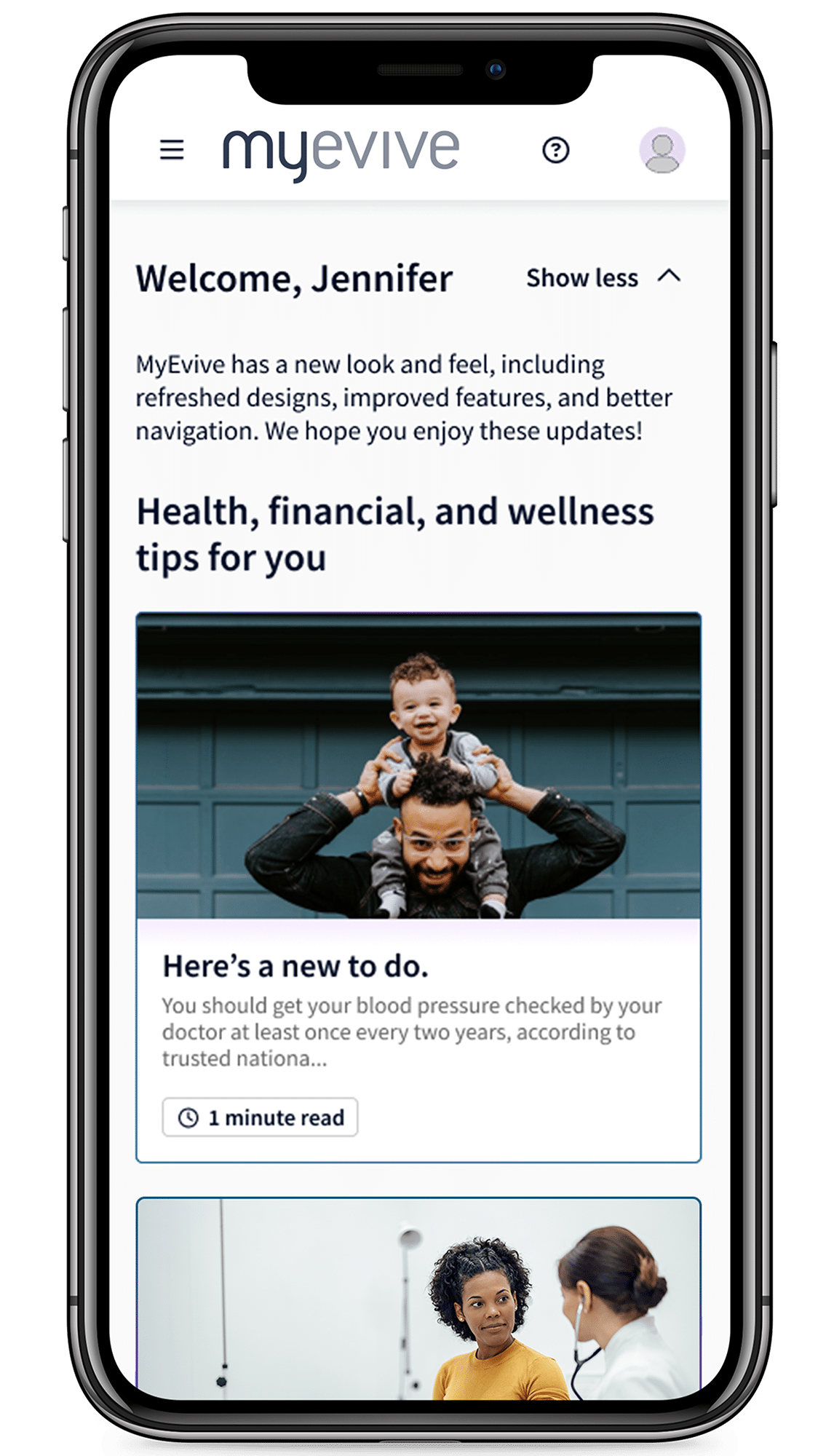
Engagement is hard. Evive makes it easy. Tour our flexible SaaS solution to learn how we simplify communications, drive better benefits utilization, and deliver measurable results with data-driven personalization and expertly curated content.